If you are experiencing pain or discomfort during sex or are finding it difficult to insert a tampon or undergo a pelvic exam, you may be wondering what the heck is going on. Maybe your doctor mentioned the word vaginismus, but didn’t offer you much information on what it is or how to go about it. Despite your doctor’s lack of information, Vaginismus is more common than you may think, with some saying between 7-22% of women experience it. Physically, vaginismus presents as painful penetration but it can also be accompanied by emotional and psychological factors such as fear, shame, or guilt. In this article, we’ll answer some common questions and fears you may have, as well as provide information on symptoms, causes, and treatment options.
Many women who’ve come to me with complaints of painful sex ask:
- Will I ever be able to have pain-free sex?
- Am I the only one who can’t have intercourse?
- Will I ever be able to get pregnant?
The answer is you are not alone, you can work towards pain-free sex, and so many women who’ve experienced vaginismus go on to get pregnant. Many have never met anyone else who has experienced painful sex, and any advice they’ve received has either lacked compassion or grossly misunderstood the situation.
What is Vaginismus?
Vaginismus is a condition that affects millions of women worldwide. It can be a challenging condition to manage, but there is hope. Comprehensive treatments are available and majority of women are able to heal completely.
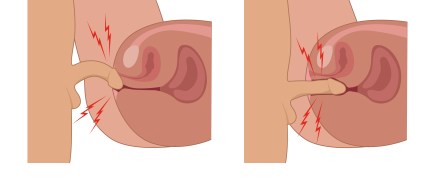
Vaginismus is characterized by involuntary muscle spasms in the pelvic floor muscles, which can make intercourse or pelvic exams painful or impossible. It can be caused by physical, emotional, or psychological factors and can be treated with a comprehensive approach that addresses both the physical and emotional aspects of the condition.
Common Symptoms of Vaginismus
These involuntary vaginal wall spasms can make it difficult or impossible to insert anything into the vagina, including a tampon, penis, or speculum. Many say that it feels like theres a wall blocking off entry into their vagina. It’s a condition that can seem elusive and difficult to comprehend. Common symptoms include:
- Pain or discomfort during penetration
- Burning or stinging sensation during sex
- Fear or anxiety around sex or pelvic exams
- Inability to or increased pain with inserting tampons or undergoing a pelvic exam
- Tightness or pressure in the pelvic region
- Difficulty achieving orgasm
- A “hitting the wall” sensation

It’s important to note that vaginismus is an involuntary reaction to penetration. The pelvic floor muscles are overreacting to a perceived negative situation at a subconscious level. Trying to “will” our muscles into behaving and relaxing during penetration might be near impossible without targeting interventions.
Things that can make vaginismus worse:
- Forcing intercourse or penetration
- Living a high-functioning / high-stress lifestyle
- Kegel exercises and some stretching/exercise positions
- Negative associations with sex or penetration
- An unsupportive partner that invites emotional manipulation into the situation
- Fears or shame associated with body image, sexuality, or performance
Getting a Diagnosis
Fun fact, Vaginismus itself is no longer listed in the DSM. The new DSM-5 categorizes vaginismus under the umbrella diagnosis of genito-pelvic pain/penetration disorder (GPPPD). GPPPD allows for a broader diagnosis where a woman must have recurrent and distressing difficulty with one (or more) of the following for at least 6 months:
While only a healthcare provider can diagnose vaginismus, you can still start working on your symptoms even if you haven’t received a formal diagnosis.
- vaginal penetration during intercourse;
- marked vulvovaginal or pelvic pain during intercourse/attempts at intercourse
- marked fear or anxiety about the experience of vaginal or pelvic pain as related to vaginal penetration
- marked tensing of the pelvic floor muscles during attempted vaginal penetration
It’s essential to understand that while seeking medical help and a formal diagnosis is important, not everyone has access to a healthcare provider who can provide answers or a diagnosis. This should not stop anyone from taking the necessary steps towards recovery. There are several ways to start working on the symptoms of vaginismus and to start gaining control of your pelvic floor muscles (see treatment options below).
Possible Causes of Vaginismus
Physical factors:
- Increased tone or tightening of pelvic floor muscles (physiological nature, trauma, sports, or child birth)
- Infections to the pelvic region
- Menopause or hormonal imbalances
- Vulvodynia, endometriosis, or other chronic pain conditions
- Some cancers or chemotherapies
Emotional or psychological factors may include:
- Anxiety or fear around sex
- Trauma or sexual abuse
- Negative beliefs, shame, or messages about sex
- Relationship issues or communication problems
- Performance anxiety, particularly in the bedroom
- Religious teachings or purity culture
Fears Surrounding Vaginismus:
It’s common for individuals with vaginismus to feel ashamed, embarrassed, or isolated. They may worry that they are the only ones experiencing this condition or that there is something wrong with them. Other fears may include:
- Fear of penetrating pain: from previous pelvic exams, tampon use, or expectation of pain. Often virgin women are told their first time can be painful. This leads to a tensing and clenching of the body as it “braces for impact” which therefore causes pain and spasming of the pelvic floor and activates a vicious cycle of anticipation of pain and then experiencing pain.
- Fear of the size of a penis
- Fear of being unable to have children
- Fear of not being able to satisfy a partner sexually
- Fear of never being able to have pain-free sex
Treatment Options
While vaginal trainers, or dilators, are often recommended as a treatment for vaginismus, a comprehensive approach is needed to achieve lasting results. This includes addressing physical factors such as muscle tension and trigger points, as well as emotional and psychological factors such as anxiety, negative beliefs about sex, and relationship concerns. Nervous system realignment, desensitization techniques, and graded exposure approaches provide some of the most research-supported and comprehensive approaches to recovering from vaginismus.
- Pelvic floor physical therapy to address muscle tension and trigger points
- Cognitive-behavioral therapy to address negative beliefs about sex and anxiety
- Couples therapy to improve communication and address relationship issues
- Mindfulness and relaxation techniques to reduce stress and promote relaxation
Hope for Vaginismus
If you are experiencing vaginismus, know that you are not alone. It\’s important to connect with others, keep open and vulnerable communication with your partner, as well as to be patient and compassionate with yourself. With a comprehensive approach that addresses both the physical and emotional aspects of the condition, it is possible to overcome vaginismus and enjoy pain-free sex.
Pain-Free Intimacy’s Mind-Body-Sex Reset Program
Pain-Free Intimacy has developed a comprehensive and holistic vaginismus recovery program called the Mind-Body-Sex Reset. This program includes vaginal retraining and desensitization, cognitive behavioral training, nervous system regulation strategies, graded exposure, group support for resilience building, as well as provides husband-specific support and information. If you\’re ready to fast-track your vaginismus recovery, this program is perfect for you. Schedule a free consultation call for more information if this program is a good fit for you. I’m rooting for you!
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596


